Request an Appointment
Contact us today to request an appointment so you can start getting the sleep you need.
The TMJ can move in all directions- up and down, and side-to-side, making it a very unique joint in the body. There is a disc of cartilage between the jaw bone and the skull which is responsible for protecting the joint and allows smooth movement of the jaw.
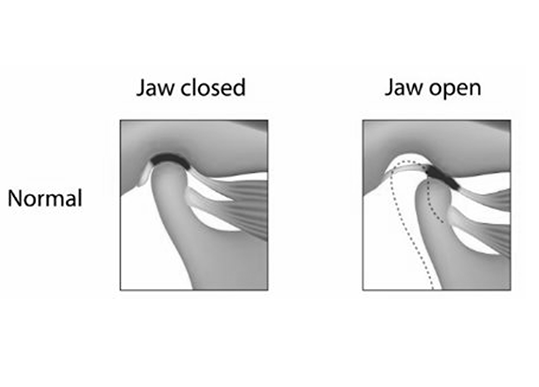
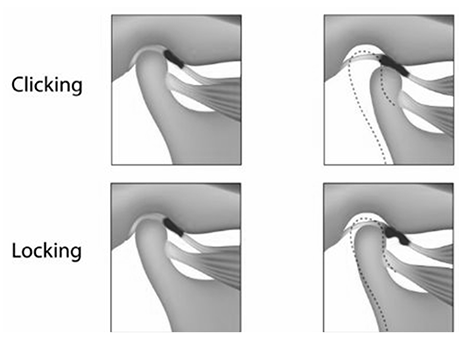
The tissues inside the jaw joint can become injured or displaced which can lead to joint sounds (clicking and popping), pain with movement of the jaw, or lack of mobility with the jaw (locking).
The bone and soft tissues of the joint can also degrade so that the bone of the jaw and skull create a grinding or crunching sound. This can occur in older individuals but may also be present in those with more systemic conditions such as rheumatoid arthritis.
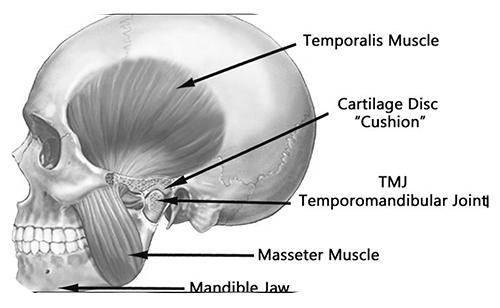
There are several muscles that move the jaw to allow for chewing, speaking, and other jaw movements. There are also muscles in the head and neck that function to support jaw movement. Like all muscles, the jaw muscles can become painful, tense, and tired from overuse or from bracing when there is a jaw joint issue. This muscle pain can also lead to headaches, especially tension headaches in the temples.
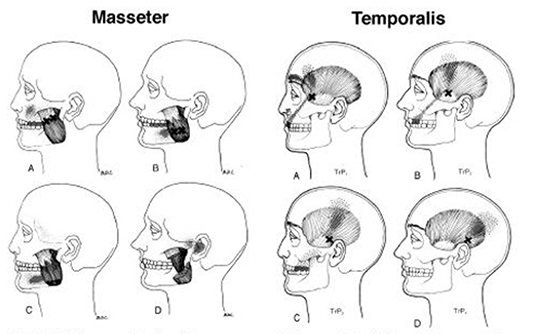
Trigger points are hyper-tensed muscles (aka muscle knots) that cause jaw aches and pains. Trigger points form as result of repetitive activity.
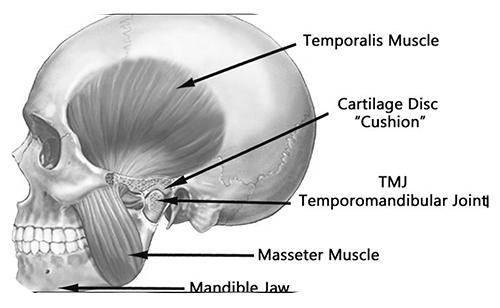
TMJ headache is head pain resulting from the pain that is first caused by tensing up of the jaw muscles then spreading to the TMJ muscles along the side of your cheeks and then reaching to the top of your head, ultimately causing a TMJ headache. TMJ Headaches can be common and sometimes are a direct result of TMJ dysfunction.
TMJ dysfunction may increase muscle tension in the jaw and masticatory muscles. e.g. temporalis, pterygoids. TMJ headaches are associate with jaw disorders. Abnormal jaw muscle tension can create TMJ disorders such as myotonic or articular disc derangements.